Retinal Detachment
 The retina is the sensory lining that covers the inside back wall of the eye. Parts of the eye such as the macula and the optic nerve are located within the retina. When an image passes through the eye, it is
The retina is the sensory lining that covers the inside back wall of the eye. Parts of the eye such as the macula and the optic nerve are located within the retina. When an image passes through the eye, it isplaced on the retina and the sensory impulses transfer the image to the brain for interpretation.
If the retina develops a tear that is not treated quickly, the retina can peel away from the back of the eye like wallpaper off of a wall. This is a retinal detachment. There are a few reasons a retinal detachment may occur. The most common is an untreated retinal tear. People who are very nearsighted have an anatomically long eye. When the eye is long the retina is stretched and can become thin and weak in some areas. Those areas can be prone to tearing and cause a retinal detachment.
Symptoms of a retinal detachment involve patients noticing a recent development of new floaters followed by loss of vision in a quadrant of the eye. A black shade, curtain or bubble completely blocks off a part of the vision. It can block the upper, lower, nasal, or temporal vision leaving the other areas uninvolved. It usually worsens without retina surgery.
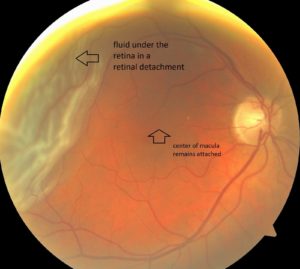
There are 2 types of retinal detachments. Macula-on retinal detachment and macula-off retinal detachment. The macula is the small central area of the retina that is responsible for detailed vision. If the retina detaches and the macula remains intact, this is a macula-on detachment. When the macula is NOT involved the prognosis for full vision recovery is usually good. If the retina detaches and pulls away at the macula this is a macula-off retinal detachment. When the macula is involved the prognosis for full
vision recovery is less predictable. Patients with macula-on detachments usually have fairly good central vision. Patients with macula-off detachments can sometimes no longer see the eye chart in the retina clinic. Dr. Stelton likes to perform surgery as soon as possible for all retinal detachments, especially macula-on detachments.
After it has been determined what kind of retinal detachment you have and to what extent the retina has detached, your retinal surgeon will determine what surgery will be needed to repair it. Typically there are 3 types of surgeries that can be performed. The first is called a pneumatic retinopexy.
With the retinal surgeon will fill the back of the eye with either an air or a gas bubble to push up against the detachment and adhere back to the wall of the eye. This procedure requires the patient to lie in a certain position (depending on where the retinal tear is) for several days to assure the bubble remains in place and pushes against the retina to secure it back in place. The bubble is then absorbed into the body on its own. The second surgery is called a scleral buckle. This is where your surgeon will use a silicone band to actually indent the back to the eye to meet the retina that has detached.
Depending on the severity of the detachment the band will sometimes wrap around the eye like a belt to secure the retina. The third surgery is called vitrectomy. Small incisions are created in the eye. A small suction and cutting device is used to remove the gel-like vitreous. Fluid is removed with suction to attach the retina. Eye gas is often used to secure the retina for 2-10 weeks to allow the eye to heal. Vitrectomy is the more common procedure of the three options. Sometimes scleral buckling and
vitrectomy are performed at the same time.
A dilated examination, ultrasounds, and high definition photographs will allow your retinal surgeon to determine the extent of the retinal detachment you have and what surgical procedure is best to repair it.
