Diabetic Retinopathy | Diagnosis and Treatment
Retina specialists and other eye doctors recommend a routine, yearly screening eye exam for all patients with diabetes to determine if they have any diabetic eye hemorrhages. When indicated, the blood vessels in the eyes are further imaged with ocular photography, optical coherence tomography (OCT), or fluorescein angiography (FA).
What is the first sign of Diabetic Retinopathy?
Diabetes damages the blood vessels in the retina. It usually affects both eyes and can harm patients with both Type I or Type II diabetes. The longer you have had diabetes, the more likely you are to have diabetic retinopathy. Patients on insulin are more likely to have diabetic retinopathy.
Unfortunately, diabetic retinopathy often presents without any symptoms. Many patients with early eye disease are picked up on routine, screening eye exams after being sent to the ophthalmologist by their primary care provider. In the late stages, patients can complain of blurred vision, fluctuating vision, blind spots, eye floaters, red-tinged vision, or eye pain.
What are the stages of Diabetic Retinopathy?
Retina specialists will use findings from your dilated eye exam to determine the stage of diabetic retinopathy. The stages follow a predictable pattern and treatment is indicated once you reach the last stage -proliferative disease.
- None
- Mild – small areas of balloon-like swelling of retinal blood vessels (microaneurysms)
- Moderate – more microaneurysms and deeper retinal hemorrhages
- Severe – pronounced change to eye veins, more severe vascular abnormalities, retinal hemorrhages in all parts of the retina
- Proliferative – most advanced form of diabetic retinopathy, a low oxygen environment signals the growth of fragile new blood vessel which may leak blood into vitreous cavity
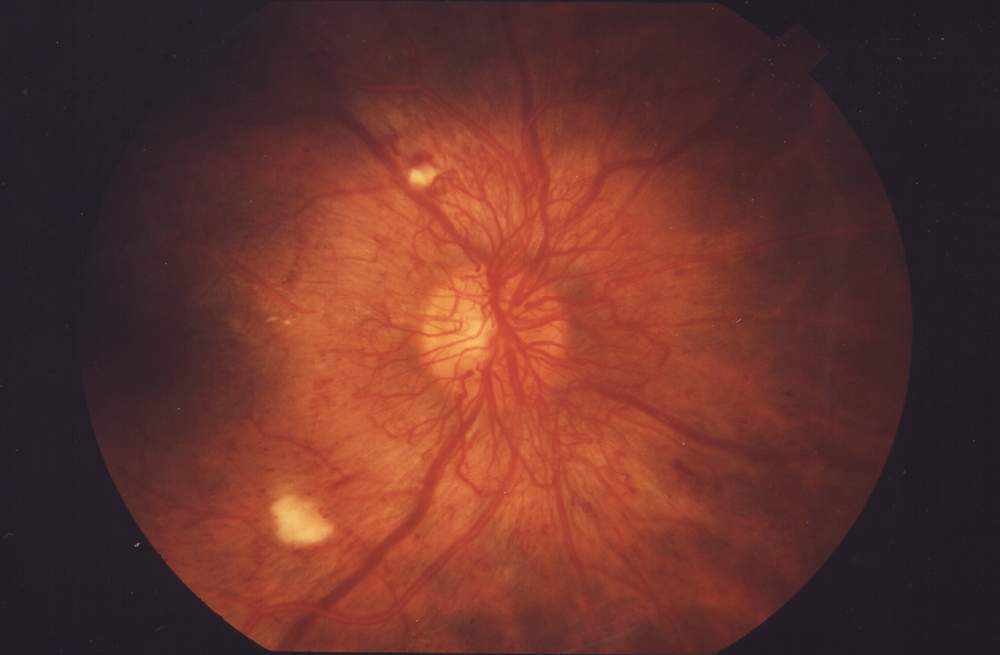
note the abnormal blood vessels over the surface of the optic nerve and retina, if they bleed the whole eye can fill with blood (i.e. vitreous hemorrhage)
Can you cure Diabetic Retinopathy?
Panretinal photocoagulation (PRP) or eye injections can be used to slow, and often halt, the progression of proliferative diabetic retinopathy. Vitrectomy or laser eye surgery is often not needed and is reserved for the most advanced cases. Patients with diabetic eye disease may also have macular edema which is easily treated with painless eye injections.
The best “treatment” for most patients is early detection. Many patients can avoid the damage that occurs to an eye in the proliferative stages if retinopathy is detected in the early stages. Your eye doctor will alert your primary care doctor to the need for good blood pressure and blood sugar control when necessary. As with most eye conditions, the earlier you receive treatment the less likely you will suffer any permanent vision loss from diabetic retinopathy.
